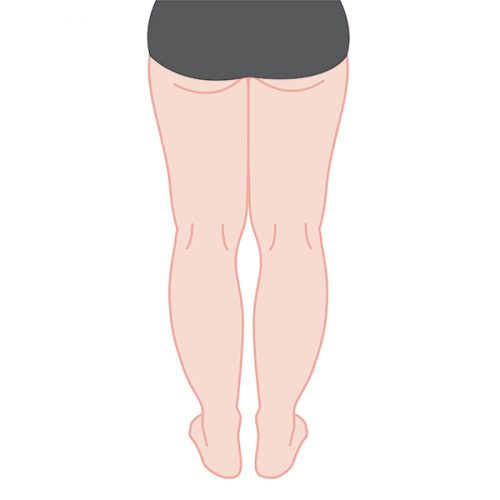
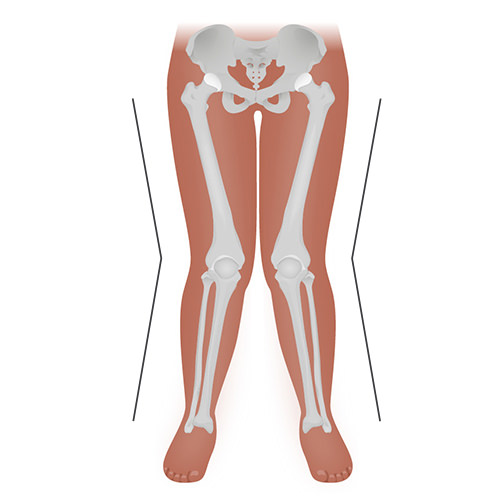
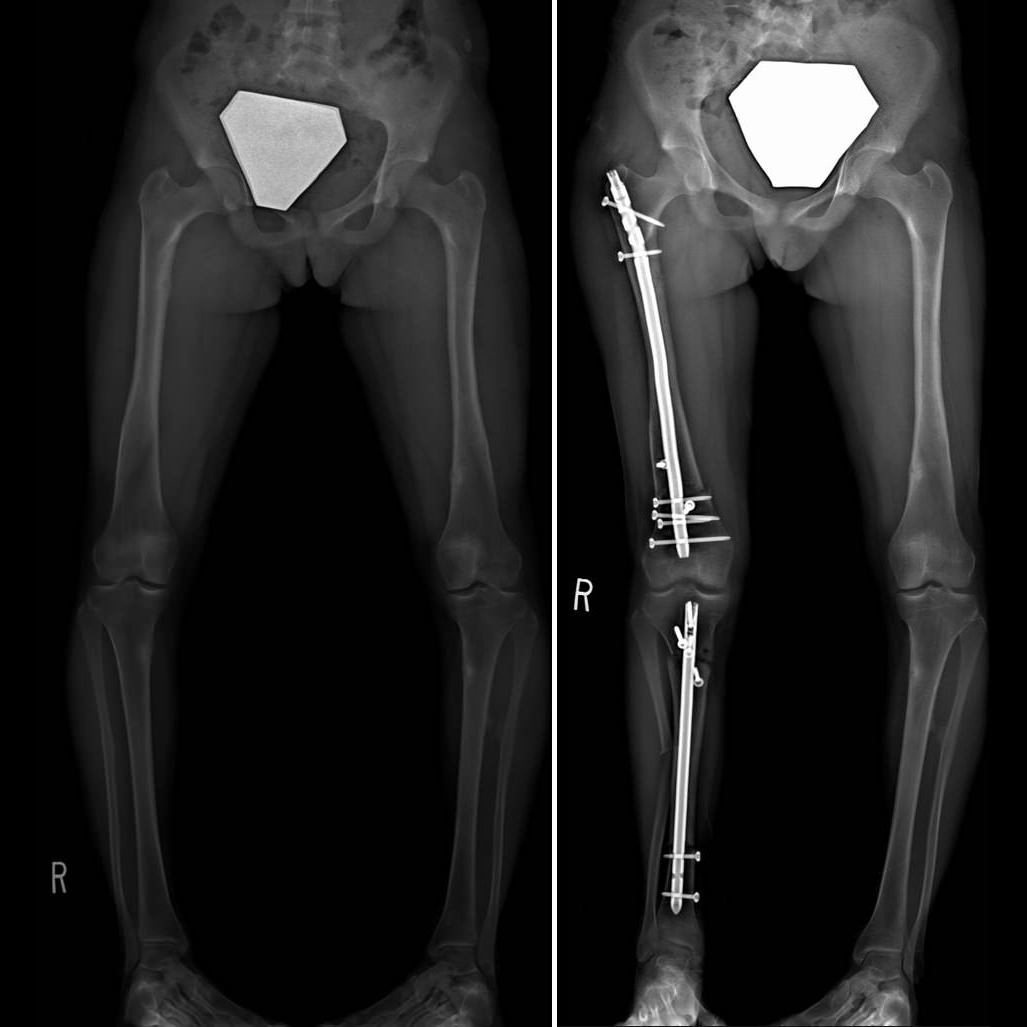
WELCOME TO CANADA’S FIRST SPECIALIZED CENTER
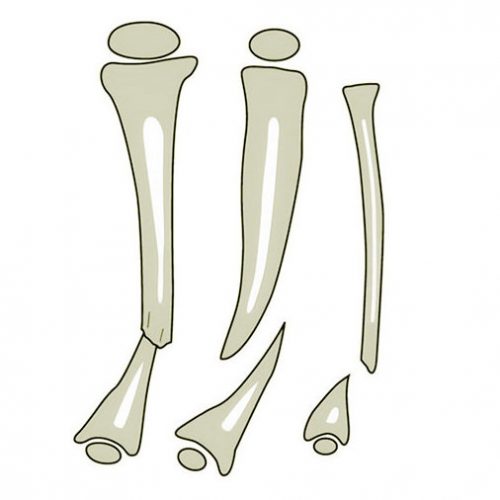
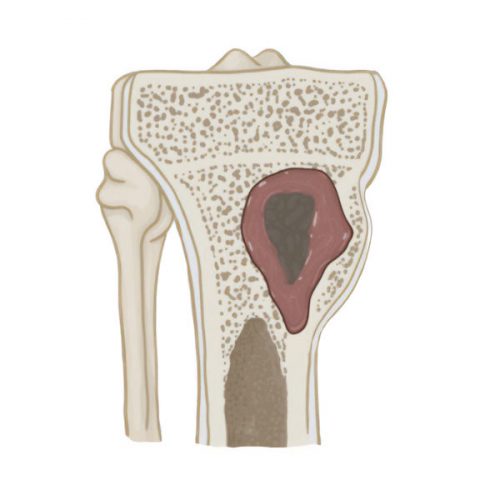
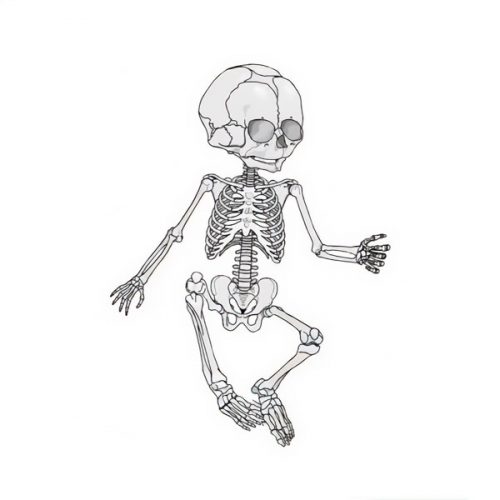
in limb lengthening and deformity correction for both pediatric and adult patients.
Canadian Limb Lengthening Center is one of the leading orthopedics centers in Canada where orthopedic surgeons, physical therapists and rehabilitation specialists
work together, adopting a patient-centered care approach and providing cutting edge technologies.
We are here to help you to achieve your long-lasting dreams.